Impingement syndrome
Shoulder impingement / subacromial impingement / painful arc syndrome
In the case of impingement syndrome, tissue that is located beneath the roof of the shoulder becomes impinged between the head of the humerus and the shoulder roof. The pain that occurs is felt primarily when elevating the arm.
The word 'impingement' is a confusing term. The literal definition is 'collision', but in the case of impingement syndrome it usually means 'trapping'.
Description of the condition
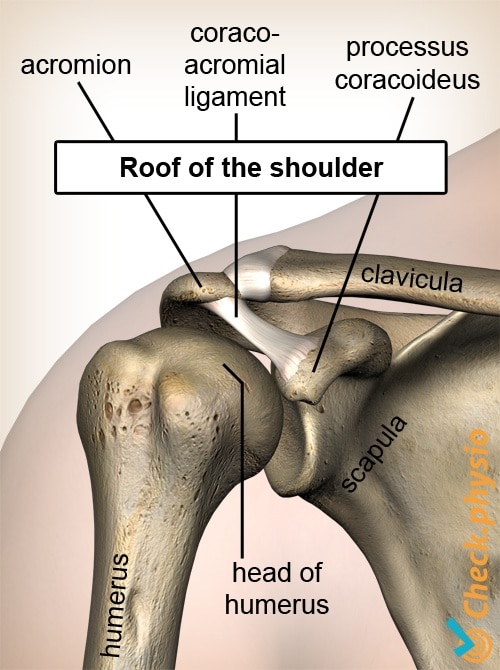
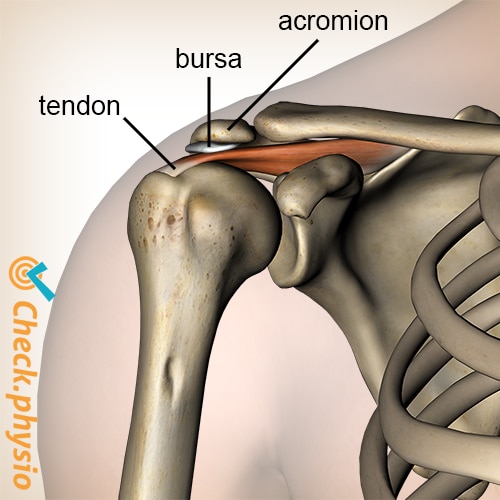
The shoulder joint consists of structures such as the shoulder blade and the upper arm bone (the humerus). The roof of the shoulder is formed from the shoulder blade and consists of the acromion, the coracoacromial ligament and the coracoid process. The roof of the shoulder is located above the head of the humerus.
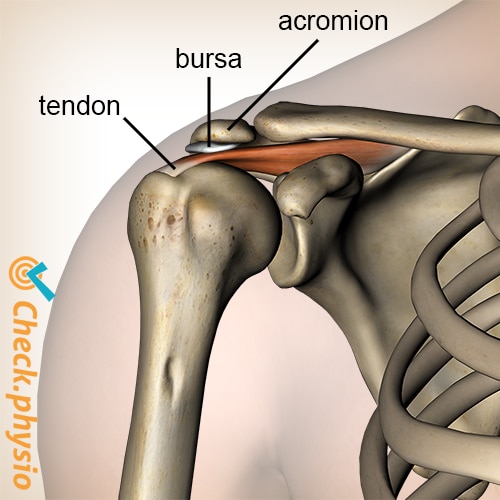
There are muscles, tendons and bursae located between the roof of the shoulder and the head of the humerus. In the case of impingement syndrome, one or more of these structures become trapped because the head of the humerus moves too far upward against the roof of the shoulder. There are various causes.
Cause and origin
Firstly, the impingement can be caused by certain structures under the roof of the shoulder swelling or taking up extra space. This results in impingement more rapidly when the upper arm is elevated.
A second cause is that the space under the roof of the shoulder becomes smaller because the humerus moves too far up. This can be caused, for example, by incorrect functioning of the 'rotator cuff' muscles in the shoulder.
The roof of the shoulder can also have an unfavourable shape, making the space below (the subacromial space) smaller and thus leading to more rapid impingement.
Signs & symptoms
As impingement syndrome can have various causes, the symptoms can differ for each patient. Typical characteristics are pain on the outside of the shoulder, sometimes radiating to the upper arm and in severe cases to the hand.
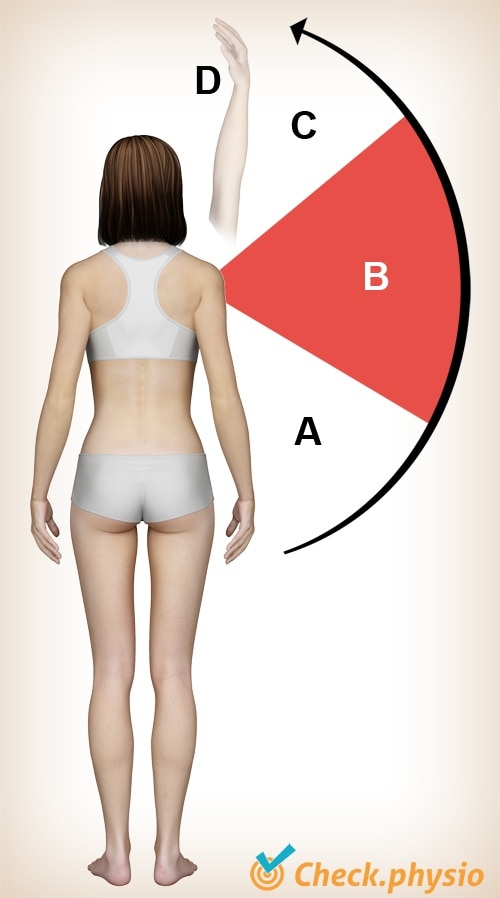
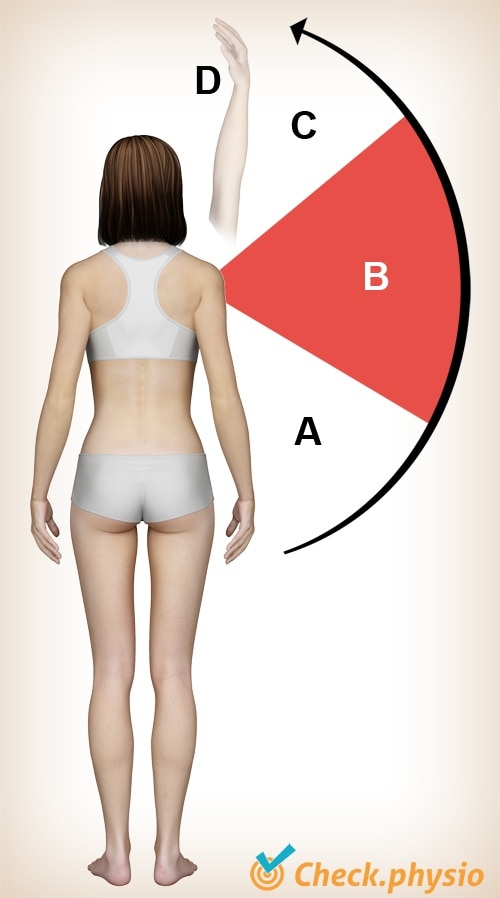
The pain occurs when elevating the arm. This is often felt in the range of movement around 90 degrees (see image, movement range B). The end of the movement can also be painful. In addition, the patient experiences pain during rotational movements of the upper arm and when elevating the upper arm against resistance.
Diagnosis
The diagnosis of impingement syndrome can be made by a physiotherapist, general practitioner or orthopaedic doctor. The diagnosis is made on the basis of the history of complaints and the results of the physical examination. During the physical examination, the cause of the impingement syndrome is also examined. If tendon problems are suspected to be the cause, an ultrasound can be requested. An ultrasound examination can also be used to rule out other conditions. Further additional testing is not necessary to make the diagnosis.
Treatment
The treatment is aimed at reducing the pain and improving the mobility and muscle function. The aim is to increase the subacromial space and thus relieve pressure on the affected structures. Training the rotator cuff muscles can play an important role in this process. In addition, stretching exercises can be used to normalise the muscle length of shortened muscle tissue.
If (acute) severe pain is the main problem, the GP or specialist can decide to administer a corticosteroid injection (anti-inflammatories).
Depending on the nature and the aim of the treatment, the physiotherapeutic treatment is expected to have an effect on the pain and/or the mobility within 3 to 6 weeks. Surgical intervention can be considered if this is not the case, an injection does not provide relief and the symptoms are severe.
Exercises
Follow the online exercise programme here with specially designed exercises for impingement syndrome.
You can check your symptoms using the online physiotherapy check or make an appointment with a physiotherapy practice in your area.
References
Hyvönen, P. (2003). On the pathogenesis of shoulder impingement syndrome. Oulu: University Press.
Jansen, M.J., Brooijmans, F., Geraets, J.J.X.R., Lenssen, A.F., Ottenheijm, R.P.G., Penning, L.I.F. & Bie, R.A. de (2011). KNGF Evidence Statement. Subacromiale klachten. Supplement bij het Nederlands Tijdschrift voor Fysiotherapie. Jaargang 121, nr. 1.
Nugteren, K. van & Winkel, D. (2007). Onderzoek en behandeling van de schouder. Houten: Bohn Stafleu van Loghum.
Verhaar, J.A.N. & Linden, A.J. van der (2005). Orthopedie. Houten: Bohn Stafleu van Loghum.